More sample content will be posted. You can also view it on my posts on LinkedIn, and my accounts on Instagram/threads (@DwightCollmanMD).
The most focused and rigorous prep for ABEM Part I/II/ConCert Exams +AOBEM Exams +BCEM Exams
More sample content will be posted. You can also view it on my posts on LinkedIn, and my accounts on Instagram/threads (@DwightCollmanMD).
📘 **”The Complete EM Board Prep” – Your Path to Excellence in Emergency Medicine**
Welcome to the pinnacle of emergency medicine preparation! “The Complete EM Board Prep,” a meticulously designed, 1192-page masterpiece by Dr. Dwight Collman, MD, is your guide to prepare for board certification in emergency medicine.
🌟 **A Journey of Expertise**
This resource has a rich history dating back to 1989 when the groundbreaking “Oral Board Tutorial!” program took its first step. Since then, it has evolved organically to include the transformative 8-Day Interactive Review, Both are now wrapped into this latest edition. Dr. Collman, with 4+ decades of expertise, combines invaluable study advice with meticulously crafted clinical test items (TIs) tailored for the qualifying, oral, and ConCert™ examinations.
🔍 **A Balance of Comprehensiveness and Precision**
Dr. Collman’s mission is crystal clear – to strike a perfect balance between comprehensive content and laser-focused study materials. In the ever-evolving medical landscape, this text evolved in tandem. Its relevance extends beyond board certification, catering to all emergency medicine practitioners as it serves as an essential companion for clinical practice.
📚 **A Treasure Trove of Knowledge**
This invaluable resource employs a quick-reading format, offering pearls of wisdom spanning several chapters, rapid test items, detailed clinical test items, oral exam case simulations, pictorial items, and key outlines from the Study Guide. Dr. Collman’s years of dedication to creating medical illustrations enhance your understanding of complex pathophysiology.
🗺️ **A Journey of Excellence**
Section I offers an essential introduction that provides invaluable study advice, guiding you through the process of focusing and skillfully applying your clinical knowledge for the board examinations.
Section II contains hundreds of rapid test items meticulously categorized into various medical content areas, guiding you to excel in the qualifying and ConCert examinations.
Section III is additional dedicated space for comprehensive preparation for the ConCert exam, presenting clinically-oriented sample questions in intricate detail.
Section IV – the Oral Board Tutorial – demystifies the examination process, offering insights into his approach to each case simulation, case documentation, case interaction with the examiner, performance ratings and scoring criteria. Dr. Collman’s detailed examiner instructions guide you to maximize your case scores. Remember, he has been an oral/written exam item writer for two EM boards. He has also been employed to train examiners to present the oral examination.
Section V comprises 27 board-level case simulations, equipped with examiner notes, insights, and pearls, closely simulating the actual examination content.
Section VI offers pictorial test items that parallel the critical visual stimuli in the ABEM examinations.
Section VII includes Dr. Collman’s personal outlines, highlighting essential keywords, principles, and he includes updated drug dosing information throughout the text.
With 1192 pages of profound knowledge, “The Complete EM Board Prep” is your gateway to excellence. Dr. Dwight Collman, with decades of experience, is not just your author but your mentor, offering guidance, private tutoring , and support in your personal journey for certification, recertification and clinical excellence. His content will serve you well throughout your career.
Stay connected with Dr. Collman:
📧 Email: dwightcollman@emednation.com
📷 Instagram: @DwightCollmanMD
📱 Thread’s Account: @DwightCollmanMD
🌐 Website/blog: E-Med-Nation.blog
💼 LinkedIn: DwightCollmanMd
Your journey to board certification and excellence in emergency medicine begins today with “The Complete EM Board Prep”!
The Complete EM Board Prep!
1192 page training program for emergency physicians preparing for board certification.
$899.00
Current “The Complete Emergency Medicine Board Prep!”promotional discount pricing:
Promotional discount for residents-in-training. Please email a copy of a letter of verification from your residency program to DwightCollman@emednation.com. The complete preparation you need to prepare for certification in emergency medicine. 1192 pages. Written and illustrated by Dwight Collman, MD. This text is now available as of Nov 1, 2023.
Fee:
Standard: $899.00 U.S.
Promotional Discount Residents: $499.00 U.S.
The Complete Emergency Medicine Board Prep!
Discount for residents in training. Please email a copy of a letter of verification from your residency program to DwightCollman@emednation.com. The complete preparation you need to prepare for certification in emergency medicine. 1192 pages. Written and illustrated by Dwight Collman, MD. This text is now available as of Nov 1, 2023.
$499.00
Hey everyone! I just completed writing and illustrating my next text to prepare you for board certification and recertification. This is an 1192 page comprehensive approach to the qualifying, oral, and concert examinations. Remember, ABEM recertification is now every five years. I included thousands of questions with answers including new updated questions for each examination with pictorial items expanded in a separate chapter. If you know the content in this text you have true mastery over the core knowledge of emergency medicine. There are 27 highly detailed oral examination cases and a complete updated version of my oral board tutorial manuscript. I have also included key outlines of chapters from the study guide.
The information in this new text includes all of my updated content from both my Oral Board Tutorial and 8 Day Interactive Review programs. Over 12,000 of your colleagues have participated in these prior programs since 1989.
There are over one hundred pages dedicated to study advice, my test-taking pearls, and every detail you would ever need to pass each of the ABEM/AOBEM examinations. I even include every tip I ever taught to actual board examiners who administered the oral examination. This text will also help you perform at your peak in clinical practice. That has always been my primary goal. The price is $899.00 US for practicing physicians and $499.00 for resident physicians-in-training (please email a letter from your program for this promotional offer to me at DwightCollman@emednation.com). I can also help you with private tutoring if you require it. All updates are complimentary for the next 5 years when you purchase this eText. Please contact me personally at my email or call/text me at 561-305-8163. If I’m away from my desk please leave a detailed message with all of your contact information including your email, phone number, and a best time to reach you. You can also leave messages in the reply box (scroll to the bottom of this page). I will be happy to answer any questions. This is a significant purchase so do not hesitate to call me. I take pride in providing personal service. I never sell or release your personal information to any third party.
The Complete Emergency Medicine Board Prep!
The complete preparation you need to prepare for certification in emergency medicine. 1192 pages. Written and illustrated by Dwight Collman, MD. This text is now available as of Nov 1, 2023.
$899.00
The Complete Emergency Medicine Board Prep!
Discount for residents in training. Please email a copy of a letter of verification from your residency program to DwightCollman@emednation.com. The complete preparation you need to prepare for certification in emergency medicine. 1192 pages. Written and illustrated by Dwight Collman, MD. This text is now available as of Nov 1, 2023.
$499.00
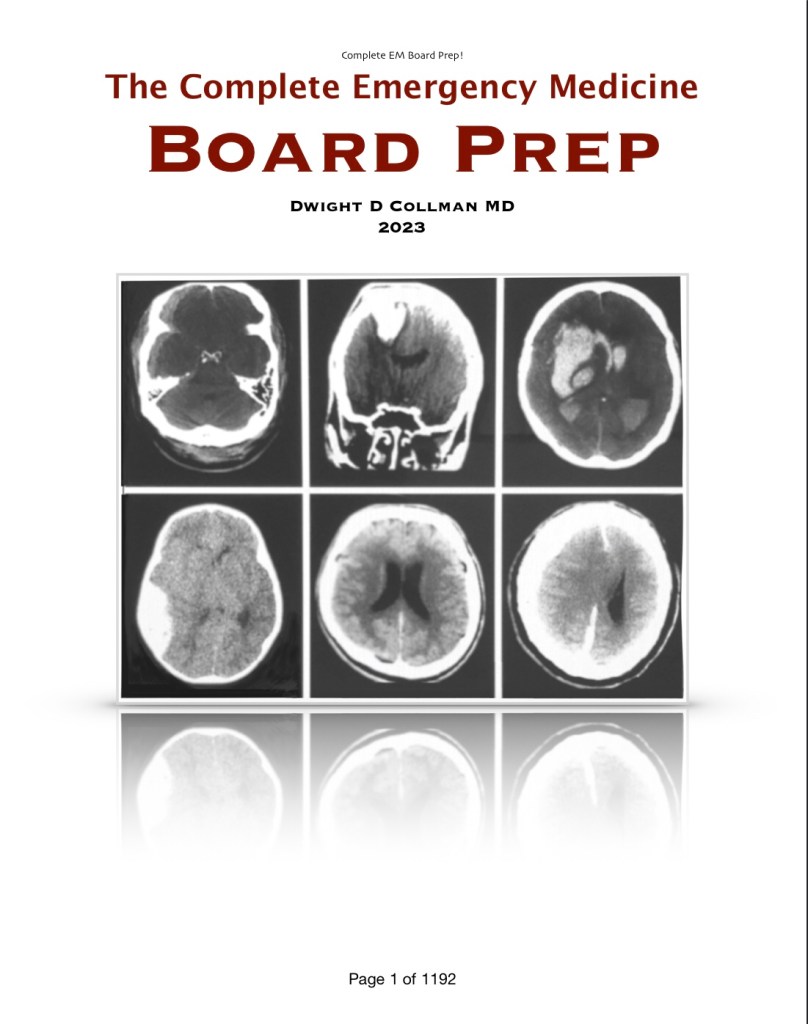
Test Item 2/multiole questions: What is the diagnosis? Describe all of the findings. Is this a pathognomonic study? What is all the indicated management?
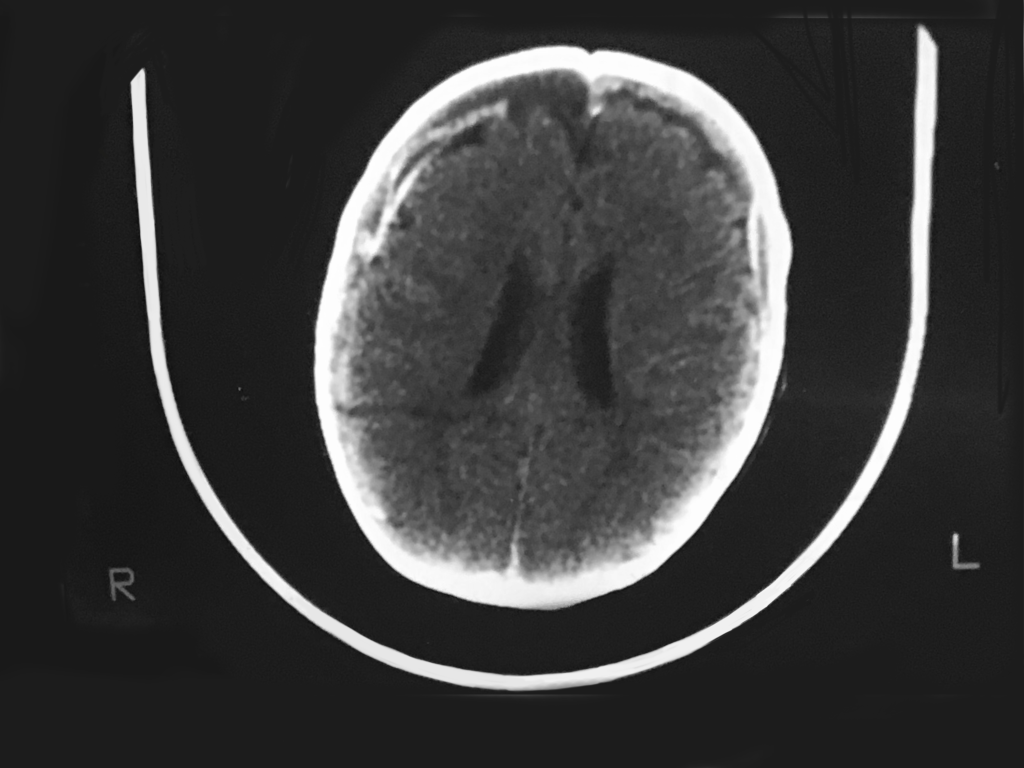
CT findings: Bilateral frontal old SDHs seen as loss of bifrontal cortical gray matter with bifrontal hygromas; acute Rt frontal SDH [white crescent on right], brain laceration on right deep within the substance of the brain [dark horizontal line rt posterior]; dilated ventricles = increased intracranial pressure.
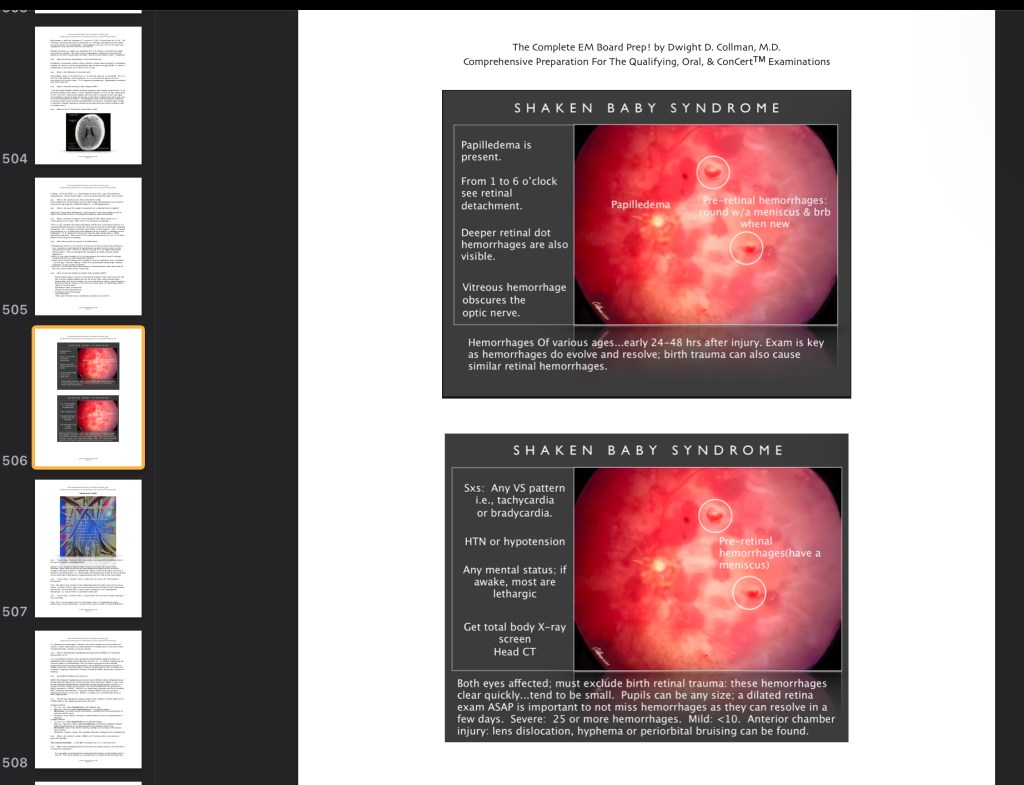
Test Item 2 Answers: Dx: This CT [-} study is pathognomonic for shaken baby syndrome!!
Management: Early Intubation and head elevation with cervical spine protection. Baseline ABG and mild hyperventilation. Frequent vital signs. cardiac/pulse ox monitoring. Possible need for loop diuretic. Establish an IV; maintenance fluid. Establish NG and foley catheters. Admission labs comprehensive T/S; U/A; coagulation profile; toxicology screening. Lateral spine film or CT neck. Chest xray. Other studies may be indicated. Call for Peds and Neurology/Neurosurgery admission. Full physical examination looking for associated injuries with attention to full neurologic examination. The patient must be fully undressed with diaper removed for the physical examination.
Bilateral retinal hemorrhages: will need a dilated ophthalmologic exam performed by an ophthalmologist (see image below).
Skeletal survey looking for multiple fractures in various stages of injury, i.e., chronic and or acute injuries of various ages. Metaphyseal corner fractures of any long bone [e.g., knee or ankle are also pathognomonic for child abuse]
Other signs of abuse: cigarette burns, grip marks or grip bruises, e.g., on upper extremities.
Call child protective services. Protect the patient from any further harm including removal from hospital.
❑ ❑ What are the 10 D’s of epiglottitis?
Dr Dwight says, “Drooling, Dysphagia, Distress = Dangerous airway! Don’t touch it! Dx and Definitive Deed (intubation) in the OR!”
The Dx is one that require a high degree of clinical acumen! Exam of the throat with a tongue blade or a flexible laryngoscope is NOT performed in the ED if the Dx is remotely suspected. The swollen flexible epiglottitis of a child can act like a ball-valve mechanism leading to acute airway obstruction if this toxic child is stressed any further!
Sample Test item 1/multiple questions. What is the diagnosis? What are the radiographic signs you see? what would you expect to find on physical examination? What is contraindicated? Is anything indicated on an emergency basis? What is the MC cause? Is there any ancillary treatment after the emergency has been managed?

Test Item 1 Answers: No this is not croup, it is epiglottitis. Signs of epiglottitis seen on this upright lateral film: Child is sitting upright in the sniffing position. The neck is straight and angled forward at the base of the neck to make the head shift forward. You see a dilated hypopharynx and can’t visualize the valecula as it is filled with swollen epiglottis. The epiglottis is oriented horizontally from edema, i.e., you see the thumbprint sign. This patient needs controlled intubation, ideally performed immediately in the operating room. On physical exam you may see a febrile, drooling child who is noncommunicative with a muffled voice and only focused on breathing, i.e., he/she is quiet. The child may be maintaining an upright posture in a tripod position and refuse to lay down while holding both arms extended at the sides. You may hear gross inspiratory stridor. Nothing should be done prior to the intubation as it may worsen the child’s condition and cause complete obstruction of the airway. If loss of the airway occurs most can initially be ventilated with an Ambu bag and mask. The next choice is needle cricothytomy and/or emergency intubation. If the child tolerates it, a face mask with oxygen can be held just in front and below the face prior to the intubation in the O.R. The MCC is S pneumoniae. Hemophlius type B was the primary cause in children prior to the introduction of the Hemophilus vaccine. However, there are periodic outbreaks of Hemophilus infections due to failure to vaccinate children. Also the most common age for this condition in children has changed from three years to eight – twelve years. Ancillary treatment: An IV line is not started until after an ET tube has been secured to avoid complete airway obstruction. Next a 3rd generation cephalosporin (either cefuroxime, ceftriaxone, or cefotaxime) should be administered and the child admitted to an ICU. A pneumococcal vaccine and/or Hib vaccine may is indicated. …from Visual Test Items [VSTIs] to be released as a new chapter section in my book The Complete EM Board Prep! © D Collman 2023. I hope to publish this text in 2023-over 600 pages! Look for it in the Fall of 2023.! Reserve your copy now!. This is everything I have ever taught or written about for 40 years to prepare you for the ABEM certifying exam, the ConCertTM exam, and the oral exam in emergency medicine. Completely updated in 2023.!
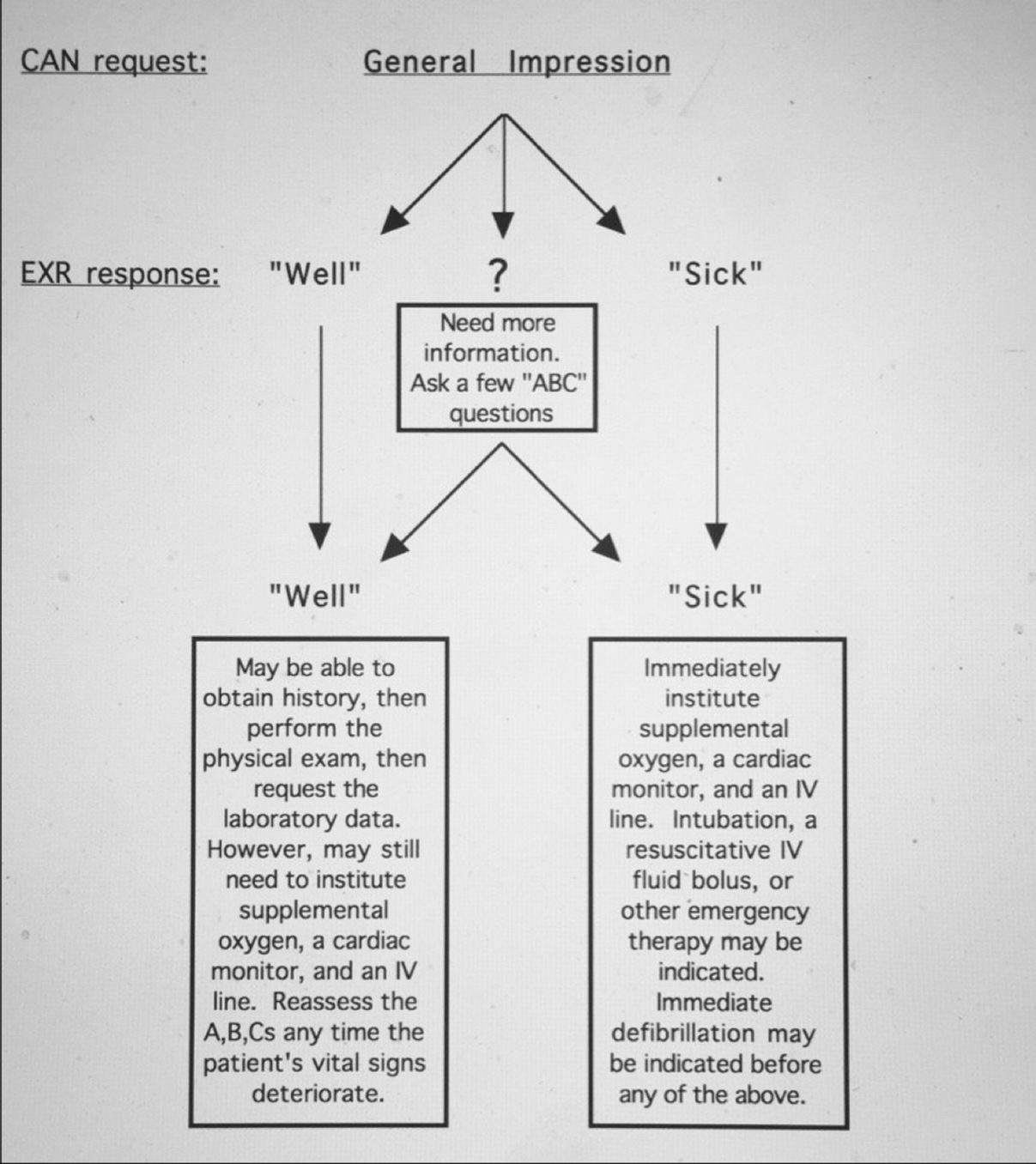
Emergency Medicine Interactive Case Management
1989-1999 D. Collman, M.D.
Diplomate of the American Board of Emergency Medicine
CASE: ANDY MICHAELS
DIAGNOSES:
• Polytrauma
SUMMARY OF THE CASE:
Andy Michaels is a 12 year-old boy who was involved in an automobile-pedestrian collision approximately 15 minutes ago and was transported to your institution by the paramedics who placed a soft cervical collar, immobilized the patient on a long padded spine board, and administered oxygen by face mask. Pt weighs 5Okg.
This child sustained multiple injuries after colliding with a car:
Airway obstruction and hypoventilation
Left pneumothorax and lung contusion.
Scalp laceration on the left occiput.
Closed head injury.
Abdominal distension secondary to a ruptured spleen.
Closed fracture of the left femur.
VITAL SIGNS:
BP: 50 Systolic (Dias. Unobtainable) P: 165 R: 50 & Noisy
PROGRESSION OF THE CASE:
This child should be managed strictly according to ATLS protocol, with initial efforts to clear the airway resulting in partial only relief of the noisy respirations. Additionaly, there is persistent hypoventilation and cyanosis. Because of this, the patient should be rapidly orotracheally intubated, after a brief period of oxygenation.
In addition, simutaneous cervical spine immobilization should be undertaken. After the patient is appropriately intubated, there is continued cyanosis and a decrease in chest wall movement and now developed breath sounds on the left hand side, due to a pneumothorax. This rapidly develops into a tension pneumothorax. This should be decompressed appropriately with a 12G in the L 2nd ICS MCL. Following this a chest tube should be placed on the left side.
Signs which the candidate may request include:
Distended neck veins.
Hyperresonance on the left side.
Diminished breath sounds on the left side.
Tracheal shift to the right.
In addition the patient is clearly in hypovolemic shock with only a palpable systolic BP of 50 and tachycardia of 175. This should be managed by aggressive fluid resuscitation with two large bore IV s, EKG monitor, type and crossmatch of the patients blood, and appropriate fluid therapy with rapid sequential 20mL/kg boluses (x 3 boluses NS or LR) plus 10 mL/kg pRBCs
The patient’s blood pressure improves minimally (60/40). Total blood volume should be estimated to be 4250cc (50 kg x 85cc/kg). Blood loss should be estimated to be at least 25% (1000-1100 cc) because of significant hypotension, and the physician should begin administration of 1/2 total blood loss as pRBCs (500-550 cc). Shortly after the onset of transfusion, the patient’s bp improves to 80/40 and the heart rate drops to 125.
Because the patient has a closed head injury (Glasgow Coma. Score-8) the patient should also be hyperventilated, with the pCO2 in the 25-30 torr range. Other appropriate therapy includes elevation of the head in a midline position, maintenance of C-spine immobilization, appropriate aggressive fluid therapy to avoid hypotension, maintenance of the airway to avoid hypoxia, and aggressive management of the patient’s systemic injuries.
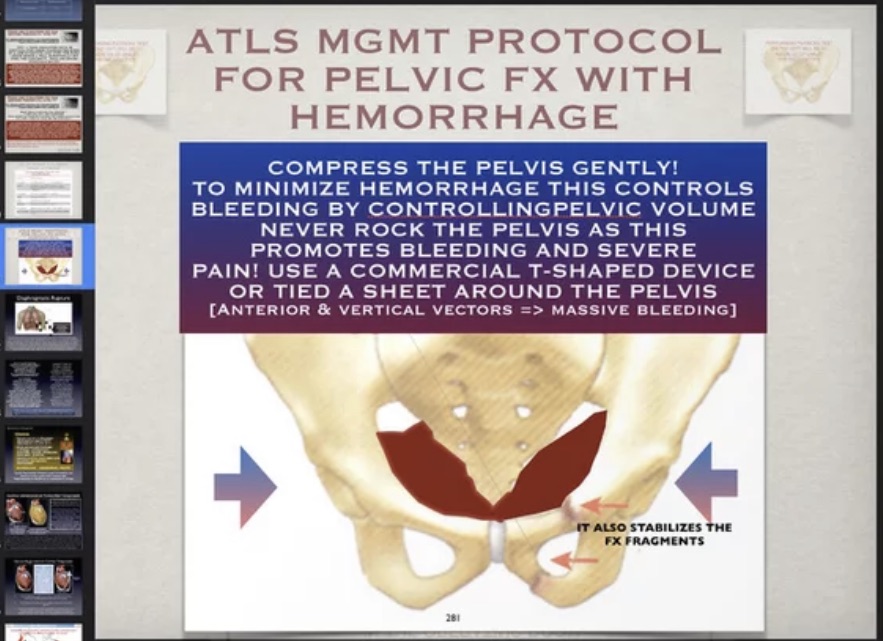
The patient also has abdominal distention, and may have a peritoneal lavage performed after the bladder and stomach are decompressed. This reveals grossly bloody fluid that is aspirated out of the abdominal cavity without lavage being performed. A bedside US FAST study, is grossly positive for free blood and negates the need for DPL if requested first. In addition there is a fracture of the left femur which requires splinting.
AMPLIFIEDD.HISTORY:
The history is not available except minimal history from a paramedic (EMT) regarding the accident.
SECONDARY SURVEY (PHYSICAL EXAMINATION):
General Impression and Mental Status:
The patient is a well developed well nourished 12 year-old male who is unconscious, but making non-purposeful movements of his extremities.
There is a dressing on the left occiput which is soaked with blood.
Skin:
Quite pale with prolonged capillary refill.
There are large abrasions on the left forearm and the left lateral thigh. In addition, there are some abrasions across the left face.
Head:
A large scalp laceration in the left occipital region, examination of the eyes shows reactive 3 mm pupils and a normal funduscopic exam. Gaze is conjugate.
Nose:
Normal.
Throat:
Normal.
Tympanic Membranes:
Normal.
Neck:
Shows no tracheal deviation or neck vein distention. Posteriorly, there is no C-spine boggyness, or stepoff deformity.
Chest:
Contusion left upper chest wall, decreased breath sounds on the left hand side, hyperresonance of the left chest and decreased chest wall rise. Following decompression of the tension pneumothorax and placement of a chest tube, breath sounds are clear and equal on both sides.
Abdomen:
Shows a slightly distended abdomen with some bruising on the left hand side.
When the left upper quadrant is palpated, there is clearly some pain there. Bowel sounds are absent. Rectal exam is normal without occult blood.
Back:
Normal.
Genitalia:
Normal.
Extremities:
There is an abrasion on the left forearm and bruising of the left thigh with marked swelling of the midthigh region. Palpation of the left thigh causes the patient react (as if he is experiencing pain).
Neurologic Examination:
The patient does not open his eyes even to painful stimuli, makes incomprehensible sounds and withdraws. He does not localize painful stimuli (GCS = 7). The remainder of the neurologic exam is unremarkable, with the exception that there is a slight decrease in spontaneous venous pulsations on funduscopic examination.
Laboratory/Xray:
CBC:
WBC: 10,800/mm3 Hgb: 11.8 G/dL HCT: 34.0%
Electrolytes/Chemistries:
Normal.
Urinalysis:
Normal.
Arterial Blood Gases:
After intubation and appropriate ventilation
p02: 200 mmHg pC02: 36 mmHg pH: 7.31
C-Spine Films:
Normal.
Skull Films:
Normal.
CXR:
If obtained prior to a needle decompression, a left tension pneumothorax is visible.
After Decompression
Shows a left pulmonary contusion. The left lung has Re-expanded.
Abdominal Films:
Normal.
Extremity Films:
Normal with the exception of the left femur film, which demonstrates a midshaft fracture.
CT Scan of Head:
Diffuse cerebral hyperemia but no mass lesions. CT scanning should be available only after appropriate resuscitation and consultation with the neurosurgeon. Results are available only if the emergency physician accompanies the patient.
CT Scan of Abdomen:
Transverse fracture of the spleen. CT scanning may be available only after an appropriate fluid resuscitation
POSSIBLE CRITICAL ACTIONS:
Airway intervention in tandem with C-spine stabilization.
Recognition of hypovolemia.
Appropriate fluid/transfusion therapy.
Recognition of tension pneumothorax.
Tube thoracostomy.
Bedside FAST vs Peritoneal lavage vs. (Abdominal CT scan).
General Surgical consultation.
Hyperventilation and neurosurgical consultation/head CT.
Splinting and orthopedic referral for femoral fracture.
PATHOPHYSIOLOGY QUESTIONS:
Q: What is the appropriate initial fluid therapy for a pediatric trauma patient?
A. For mild symptoms of shock (tachycardia, decreased pulse pressure, tachypnea) 10cc/kg fluid challenge over five-ten minutes i.e., as fast as possible. Evaluate response.
For moderate symptoms of shock (hypotension, acidosis) 20-40cc/kg fluid challenge over five-ten minutes i.e., as fast as possible. Evaluate response.
For exsanguinating hemorrhage 40cc/kg LR plus pRBCs as quickly as possible.
Q: What are the initial methods of treatment of the pediatric patient with a closed head injury?
A: • Intubation/hyperventilation:
pC02 28-30 torr (reduces cerebral blood flow without undue vasoconstriction) or other complication.
• Fluid restriction:
Avoid hypotonic solutions.
• Elevation of the head (direct hydrostatic effect)
• Osmotic Diuretics:
Mannitol—Diuresis & decreases CSF production.
• Loop diuretics :
Lasix—Reduces formation of CSF.
• Barbiturates—Reduce cerebral metabolism and blood flow.
Q: What are the indications for immediate endotracheal intubation in the child with polytrauma?
A: • Any disturbance in the level of consciousness.
• Systolic blood pressure of <20 mmHg below expected normal.
• Severe facial, neck, or chest injuries.
• In addition when ABG’s are available a PaO2 ≤80 torr
Check out iPhone Skin on Society6: https://society6.com/product/altered-mental-state-c-1989-2020_phone-skin?sku=s6-13668086p13a3v742