TIPS/VOWELS Mnemonic: For Differential Diagnosis Of Altered Mental State And Coma
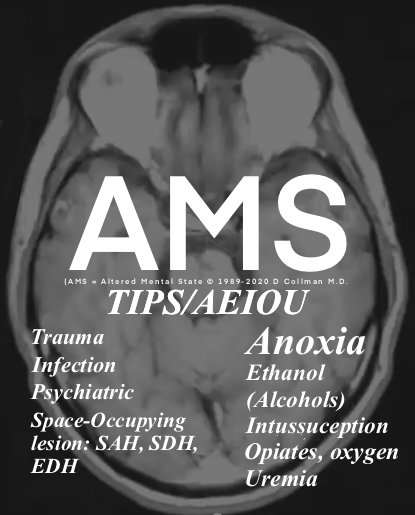
Altered Mental State [AMS]
D. Collman, M.D.
TIPS/AEIOU in detail:
T: Trauma (including polytrauma & TBI), Toxins (including ingestions or exposures that could lead to AMS). Examples: medications, recreational drugs, or environmental toxins.
I: Infection (Ex’s: meningitis, encephalitis, and sepsis).
P: Psychiatric illness may manifest as AMS: depression, anxiety, or Psychosis.
S: Space-occupying lesion (SAH, SDH, EDH, i.e., consider all forms of intracranial hemorrhage), Stroke, and Seizure (latter have various etiologies).
A: Anoxia (Anoxic encephalopathy after CPR), Acidosis, and other Acute metabolic disturbance (e.g., DKA or severe electrolyte imbalances, e.g., hypercalcemia, hypernatremia, hypermagnesmia).
E: Ethanol (include toxic alcohols: methanol/ethylene glycol), Endocrine disorder: thyroid disorders (myxedema, thyroid storm) or adrenal insufficiency.
I: Insulin (and other etiologies of hypoglycemia or severe hyperglycemia-HHS), Intussusception (latter leads to LA, pain (persistent irritability), and sepsis.
O: Opiates-Investigate the use or OD of opioid medications or substances (Administer naloxone).
U: Uremia (Assess for renal failure and associated elevated BUN/Cr levels).
Legend: LA = lactic acidosis; HHS = hyperglycemic hyperosmolar syndrome.
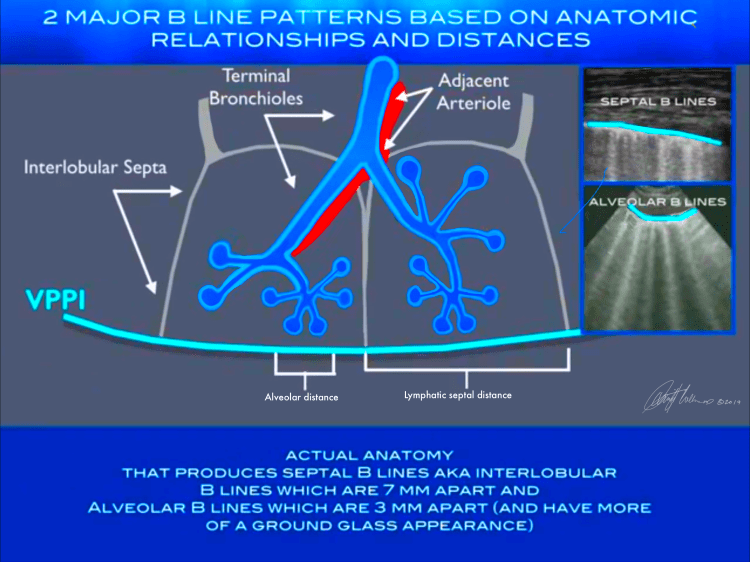
Lung Ultrasound: Septal B lines vs. Interlobular B lines

For board prep!
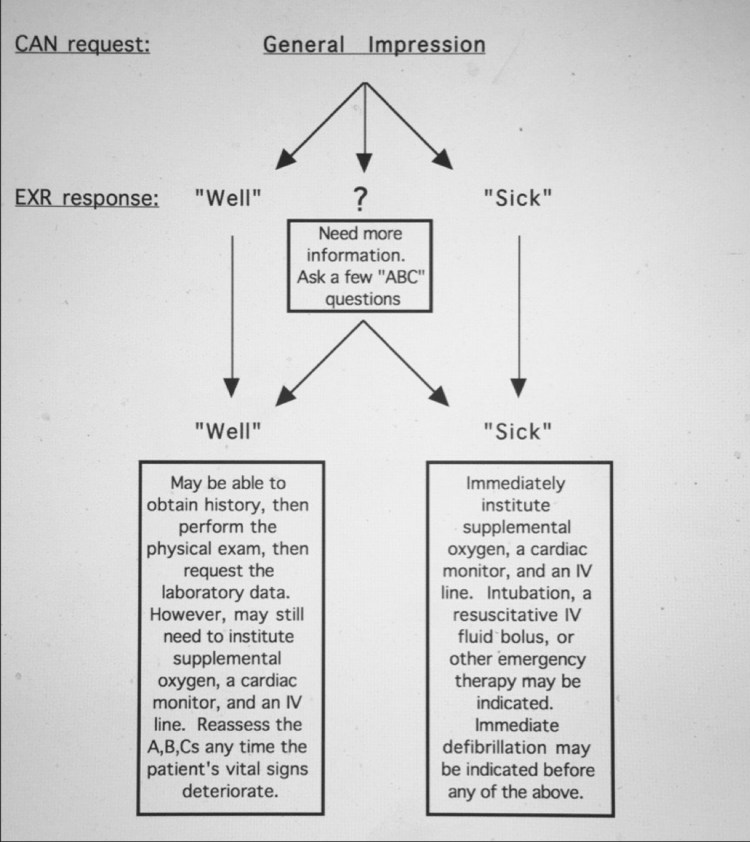
This is the simple algorithm I have presented for decades to teach the approach to all EM cases. The amount of oxygen, the types of monitors and the fluid resuscitation are personalized for each patient.
Digital art by Dr Collman including medical illustrations are available for purchase. He can create art or modify any image to your specifications. He has published art for medical texts and magazines as well produced fine art for over 50 years.
The RBC
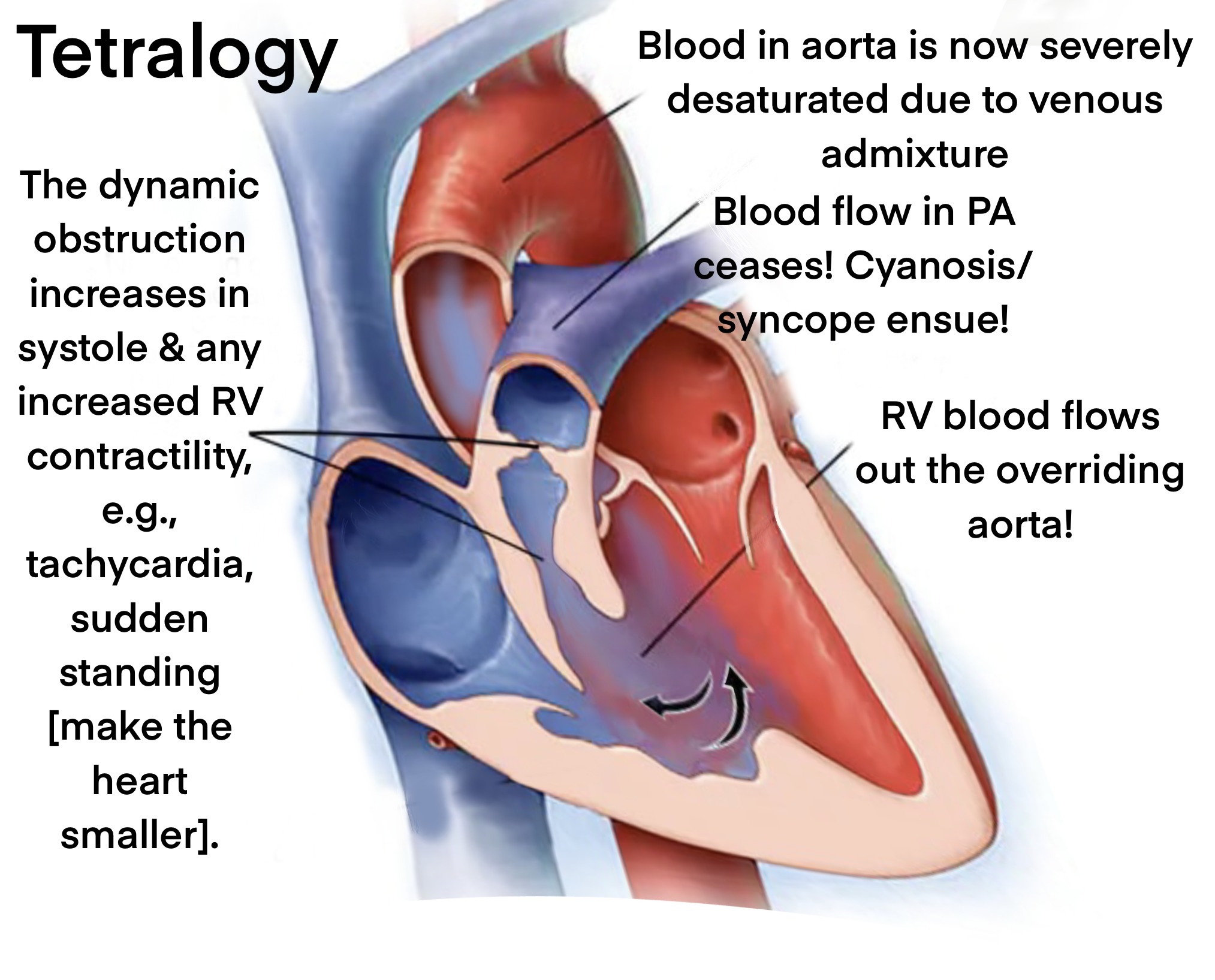
Pathophysiology/cyanotic congenital heart disease/tetralogy of Fallot-4 elements: overriding aorta, RVH, VSD, infundibular stenosis of the RV outflow tract. Illustrated:
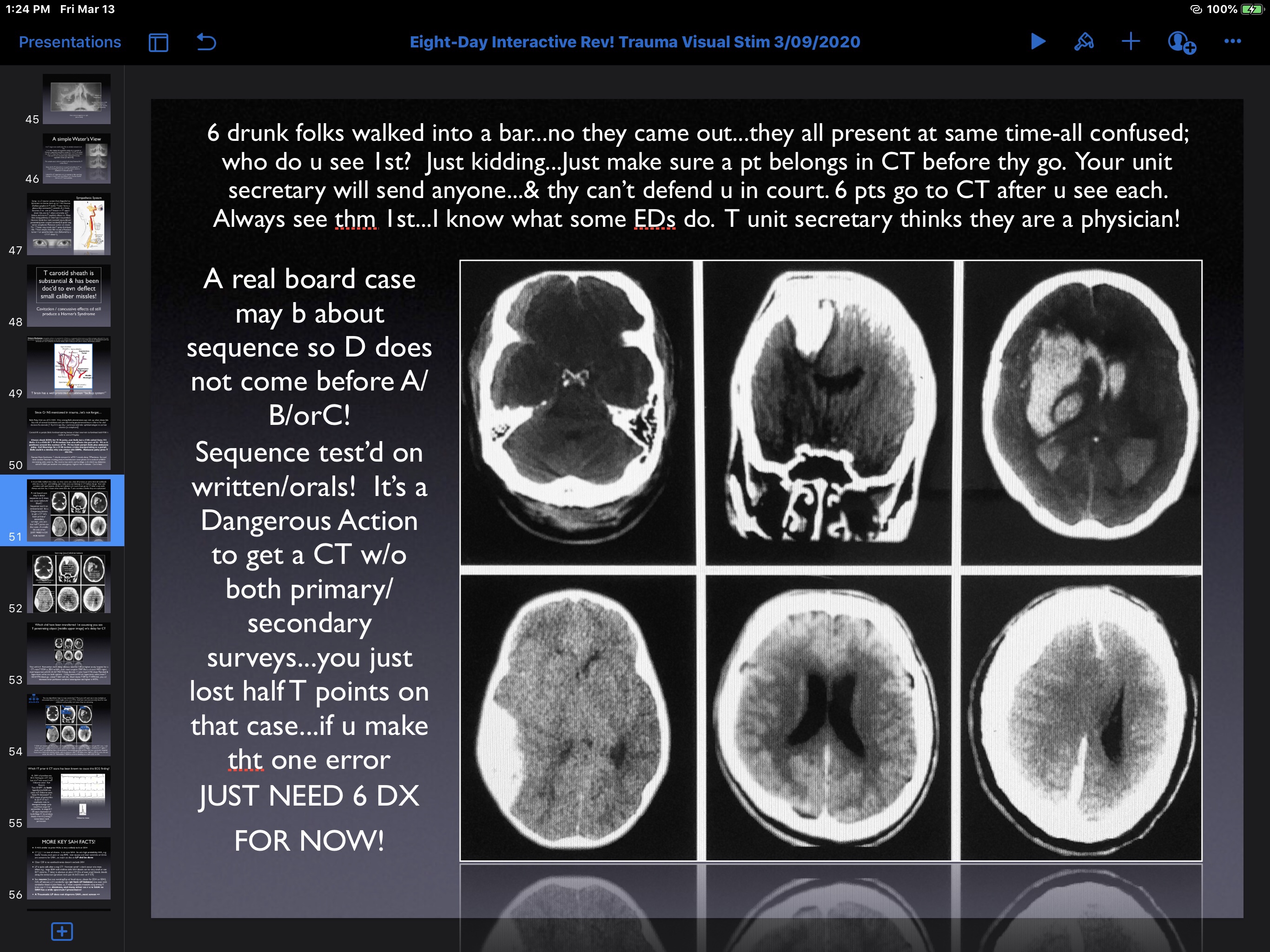
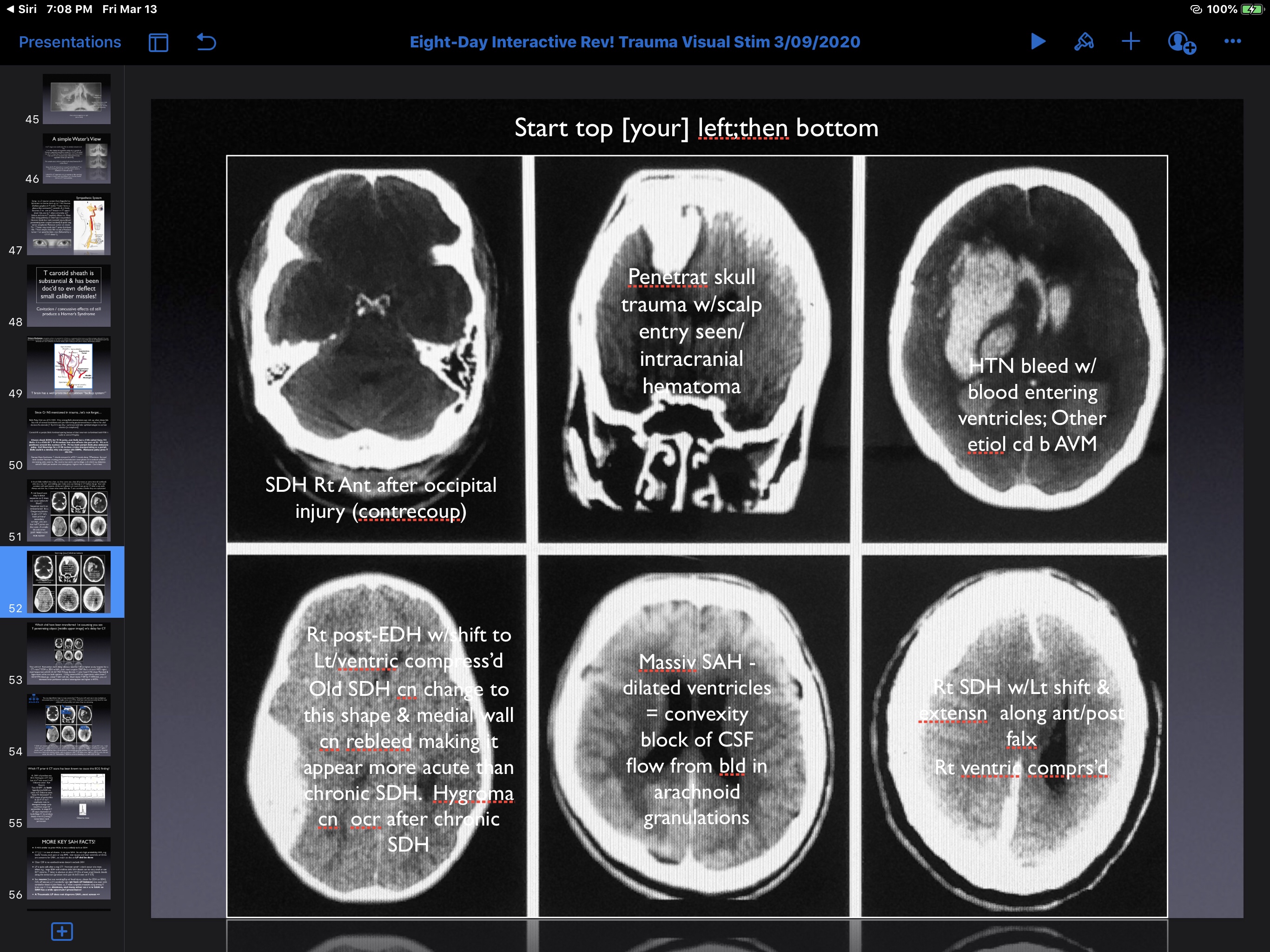
What is the diagnosis in each of these six patients? Assume they all arrive at the same time, i.e., this is a mass casualty event – How would you prioritize the overall management and transfer of any of these patients to a neurosurgeon?
Discussion: note: (On exams some images are field test items [not scored].
In this group the lower middle slice is of a patient who would likely arrive dead: he has a massive SAH that surrounds all of the cortical surfaces/even extends a long the falx in the midline [appears fuzzy due to blood filling the subarachnoid spaces immediately adjacent to the cortical sulci and gyri. The ventricles are dilated due to blood causing a CSF convexity block. So you can’t save him. The arachnoid granulations are all blocked…CSF can’t exit the head so the ICP is markedly elevated. In the midline [along the falx cerebrii] the blood appears fuzzy because it is a thin film that follows the sulci/gyri closely…it often looks like a zipper…described as the “zipper sign” and proves its a SAH along both sides of the falx. No intervention for this patient.
Next, the patient in the upper middle slice has a knife blade penetrating into the brain: traumatic penetration by knife [knife not visible on this slice] requires immediate transfer [1st] especially if no other injury. The knife should not be removed in the ED.
The upper left slice is of a patient with the lowest acuity [a right frontotemporal SDH [venous bleeding] and could be transferred last in this mass casualty simulation. However, this patient requires RSI before transfer. This patient has has midline extension and a collapsed ventricle [mass effect] which should improve w/measures to lower the ICP…treat and transfer simultaneously [urgently].
An acute epidural hematoma is due to arterial hemorrhage [lens-shape-lower left slice and generally more acute than a SDH]. The issue…if hemodynamically normal with reactive pupils [intubate/mild hyperventilation after RSI [all get RSI except the SAH…he is dead]. An EDH might even require an emergency burrhole if the patient decompensates in the ED.
Next, a patient with a hypertensive bleed [upper right slice] requires mild hypervent/transfer ASAP & might survive, but the prognosis is poor. Decades prior if there was intraventricular blood most had very low survival…this is a patient with a right-sided AVM that ruptured [comorbidity: chronic hypertension]. The danger is the BP…do not lower the BP because with chronic hypertension cerebral perfusion is reset to a higher range to maintain cerebral blood flow; it is best to gently do RSI and transfer; this patient actually survived [as did all but the patient with the massive SAH].
The six patients:

This would be a crazy [once in a lifetime] shift…and you always remember crazy! Super-emotional events cause new neuronal connections in long term memory in both the right and left hippocampus].
Legend: SDH: subdural hematoma; EDH: epidural hematoma; SAH: subarachnoid hemorrhage; ICP intracerebral pressure; AVM: av malformation; RSI: rapid sequence intubation.
What Are The 6 CASE DIAGNOSES?